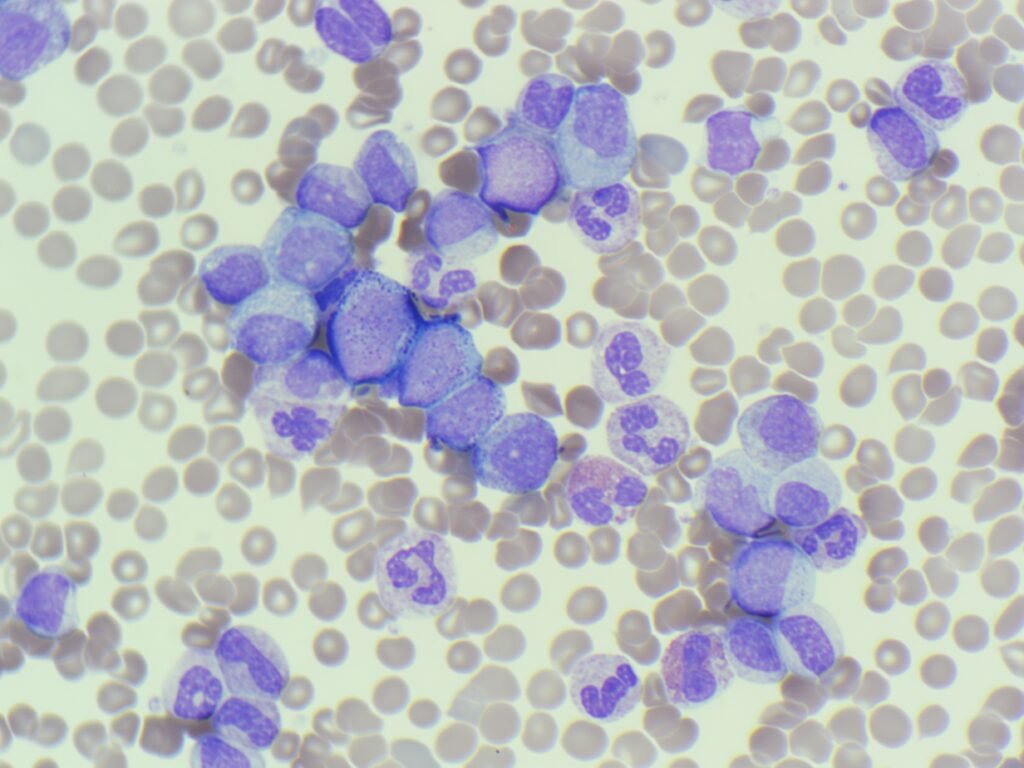
MM260126: CML
This week’s case started with a “heads-up” call from the Haematology SpR before the sample even reached the lab. The staggering WBC and the specific clinical request made for an interesting discussion.
The diagnosis: Chronic myeloid leukaemia (CML)
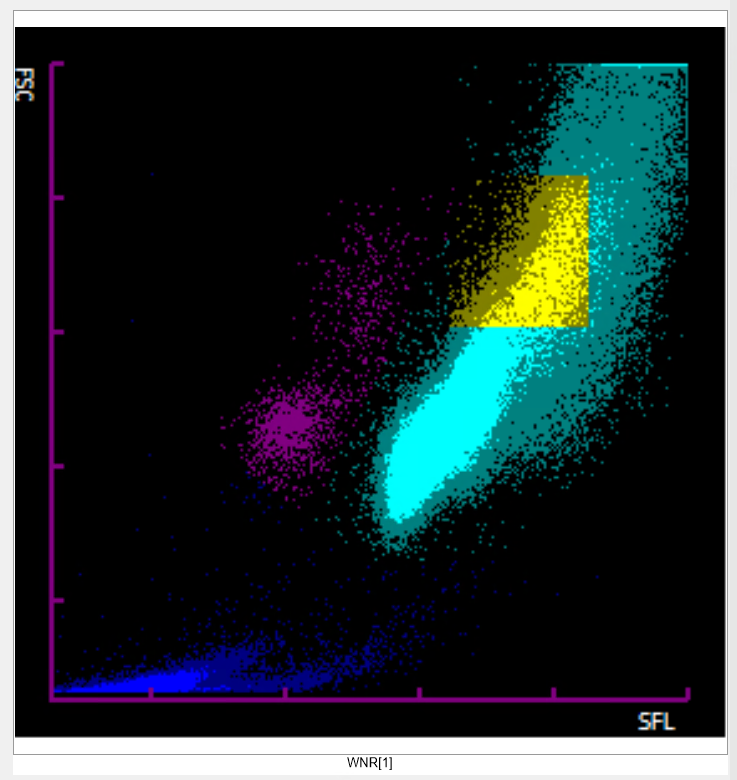
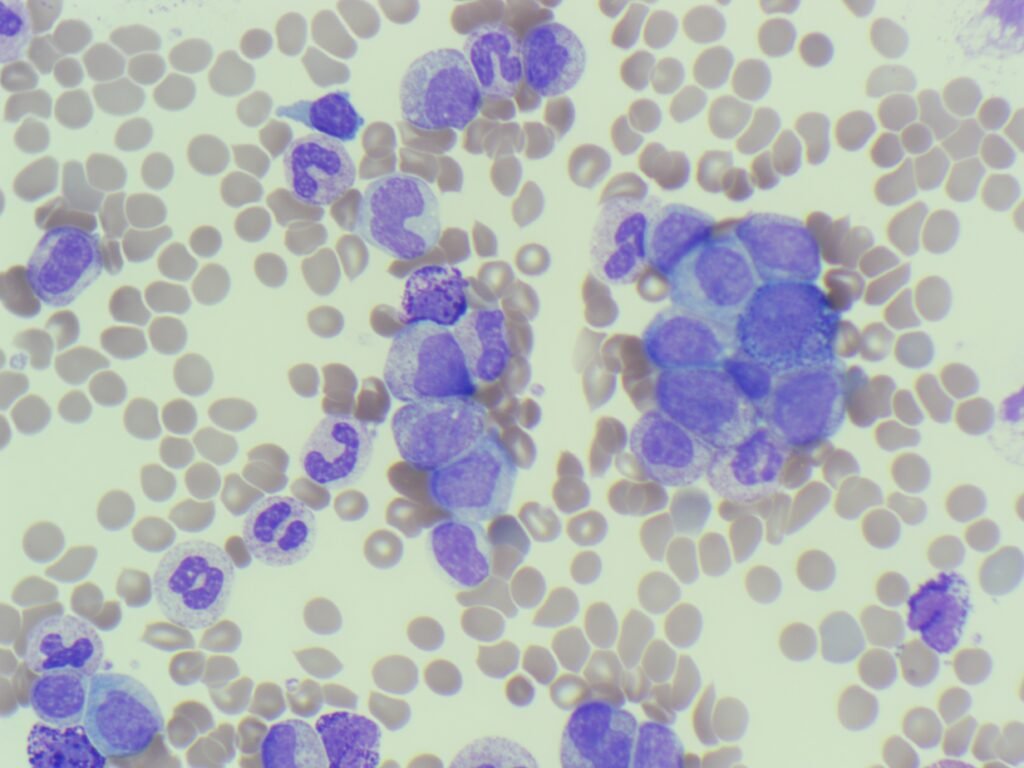
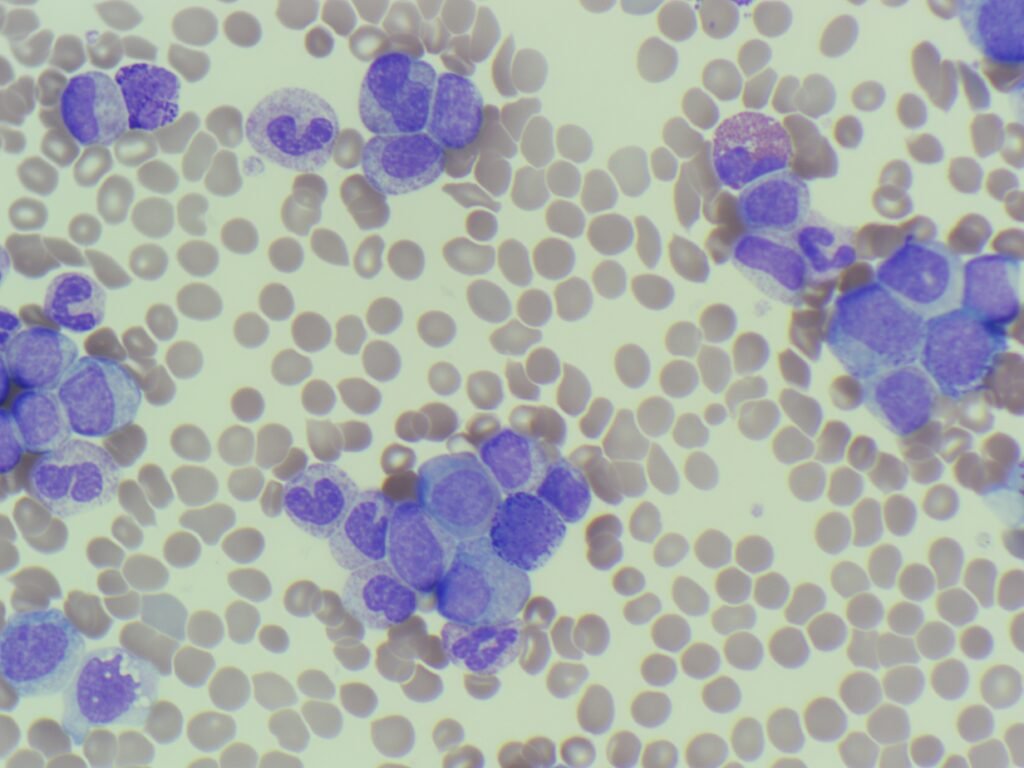
The combination of the massive leucocytosis of 319.64 x 109/L and the “garden party” of myeloid maturation, from myeloid blasts to mature neutrophils is a hallmark of CML.
The G6PD riddle: Why the urgent assay?
The most common reason a Haematology SpR requests a G6PD screen in a suspected CML case with an increased white cell count is the risk of Tumour Lysis Syndrome (TLS).
- The risk: Patients with extremely high cell turnover or a high “bulky” disease burden are at risk of TLS when starting treatment. This causes a massive release of intracellular contents, including uric acid.
- The G6PD link: The drug used for treating CML produces hydrogen peroxide as a metabolic by-product. In patients with G6PD deficiency, the red cells cannot neutralise this oxidative stress, leading to sudden and severe haemolysis and methaemoglobinaemia.
Key learning points
- Basophilia is a red flag: Significant basophilia in the presence of a high myeloid count should always trigger a search for CML or other myeloproliferative neoplasms.
- Safety first: In the emergency setting, a G6PD assay isn’t just a “test”; it’s a safety screen required before the administration of specific TLS therapies.
- Preserved parameters: Note how the haemoglobin and platelets were relatively stable despite the WBC. This is common in chronic phase CML, whereas acute leukaemias typically present with significant cytopenias.
Privacy Policy | Refund & Return Policy | Only Cells LTD © 2025