Winners and Losers
My eyes were tired. As you can tell, this is a running theme, I live in a perpetual state of tiredness. Even when I wake up I am tired. I had been staring at blood films since coming back from lunch and it was almost 6pm when the MLA can to me with a perplexed look on his face. I just wanted to go home. My back hurt. I really needed to adjust the way I was sitting and move the microscope because the twisted nature of my torso was doing nobody any good.
“It’s the haem registrar on the phone. He said something about platelets and citrates and it all went over my head. Can you speak to him please?” said the MLA.
“Sure,” I replied. I would rather have gone home but the late shift person hadn’t come back from their break. Maybe I should have called the police and lodged a missing person’s report. I didn’t even have the time nor the energy for that.
“Hello, how can I help?” I asked, quickly trying to finish the blood film comment. People always called when I was in the middle of writing one.
“Hi, I’m the haematology reg,” he began. He mentioned his name, but I was only paying enough attention to him to pick out the important bits. The rest of my attention was focused towards spelling the big word used to describe a low platelet count.
Marked t-h-r-o-m-b-o-c-y-t-o-p-e-n-a-i-s. Wait, what? Backspace, backspace, backspace, backspace, backspace.. Marked thrombocytopaenia noted, no clumps seen.
“I’ve just been contact by the haematology consultant who received a phone call from a very confused obstetric team,” he continued.
“Oh dear,” I replied, still typing; left shit to myelocyte stage with mild toxic granulation. Someone had turned off my in-built spell-checker. I went back and added the missing ‘f’.
“Can I give you a hospital number, it’ll be easier to explain?” He asked.
“Sure just give me a second,” I replied, quickly pressing the save button. The computer froze. Technology in the health service wastes many hours a day. Productivity can only be as good as the tools you have to do the work. I’m yet to come across a Trust where the basic technology, ie the computer, works as well as it should it. Random freezes and reboots are common. But that’s a story for another day.
“I’m sorry the computer is being a little sl..” just as I said it, it blinked at me, cursor in the search bar, waiting. “Okay, what’s the number?”
The registrar fumbled in his pockets to dig out the piece of paper he had scribbled it on.
“Let me find that paper I had scribbled it on. It is….”
I entered the number, confirmed whether he said s for sugar or f for flamingo and hit the search button. I could hear the hard-drive grinding. Slowly, a list began populating on the screen. This patient was obviously well known and had a long history spanning multiple years. The list continued to grow, line after line.
“Okay, so what’s the issue?” I asked.
“So this patient needs and epidural. For that, her platelet count must be above 80. But if you look at the last couple of counts, they seem to make no sense.” He was exasperated. His breathing was heavy too. Maybe he was wearing a mask like me.
I clicked. The most recent was a citrated platelet count of 52. Previous to that a standard full blood count and the platelets were 120. Going further back another full blood count with platelets of 79.
“I see what you mean,” I said reading the results out loud.
“You missed the citrated count between the two FBCs,” he said.
I looked. He was right. There was another citrated platelet with a result of 49. “Hmmmm…”
“Can you explain what is going on? Which one is accurate?”
Good question, I thought to myself. I could see why the team were confused. Apart from the two citrated counts, the two from the EDTA FBCs looked somewhat random. All the samples had been taken within the day or so. Surely there wouldn’t be so much variation in such a short amount of time. Right?
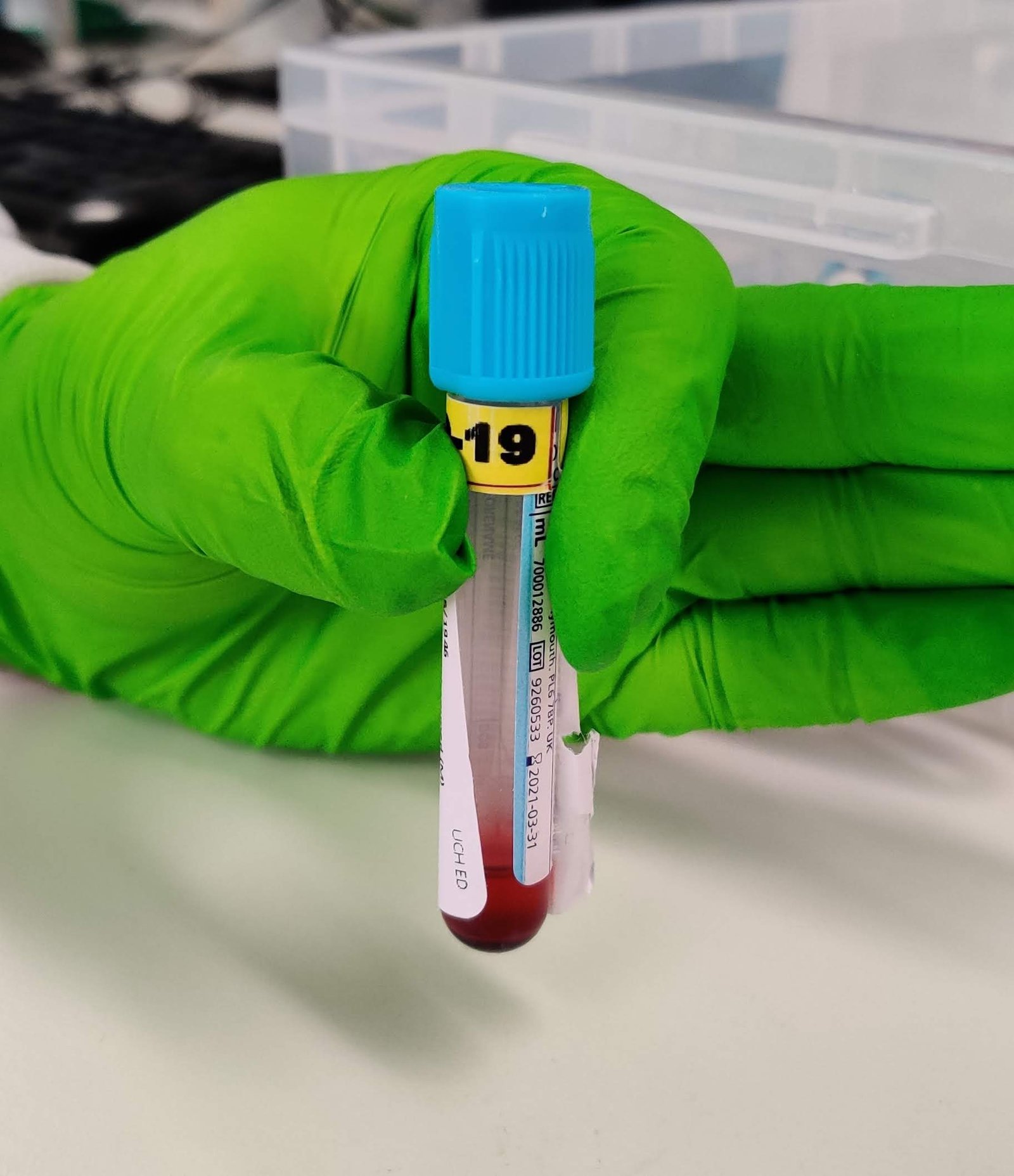
“Well firstly, the CPLT will be the least accurate, as you may be aware due to the dilution factor and subsequently our computer system does not correct for it.” I explained. Different anticoagulants behave differently. Ethylenediamine tetra-acetic acid, or EDTA as most people know it looks like a few grains of salt in the bottom of the purple top tube. Sodium citrate on the other hand is a liquid anticoagulant used in the blue top tubes. When you mix a liquid (blood) with another liquid (the anticoagulant) the total volume increases but the contents (blood cells, chemicals etc) are the same and so they are more dilute then than they were in the blood. This is why we don’t normally do blood counts on citrated samples and if any lab does do it, there is usually a correction applied to accommodate that dilution factor. Unfortunately our computer system at the time did not automatically correct for this dilution. The powers that be had determined the variation wasn’t significant enough to have the correction built into the computer system. It always irked me. All it would take was the multiplication of the raw citrated count by 1.1. This is also why the citrate tube needs to be filled to the line, as the anticoagulant is proportional to that volume. There’s a lot riding on the volume of blood being correct.
Using EDTA can sometimes cause pseudotherombocytopaenia. That’s a long word. Pseudo- means spurious, or not real. Thrombo- is to with platelets. The –cytopaenia suffix means a decreased. So pseudotherombocytopaenia in its totality means a spuriously (falsely) reduced platelet count. In some conditions platelets may be genuinely reduced whereas with EDTA the platelets can sometimes clump together and so aren’t counted properly by the analyser.
“Yes, I know that.” He said. My mind was racing. Could the FBC results in EDTA have been clotted? No there was a comment to say the samples had been clot checked and no clots were found. So that wasn’t it. I walked over to the manual filing rack and noticed a bright blue (citrate) tube in amongst a sea of purple ones waiting to be filed. Picking it up I noticed it was for the patient we were talking about. I also noticed it was half filled. The sample should have been rejected without even having processed. Ah sh*t I thought. It would have been unprofessional for me to say it out loud, no matter how much I may have wanted to at that time.
“I’m really sorry,” I apologised. “That citrate sample was underfilled and so the results given would be grossly inaccurate. That sample should not have been processed.”
“So what now?” he asked.
“The best thing would be to send another sample so that we can ensure the results are accurate. Also doing a citrated platelet count isn’t necessary as the platelets weren’t clumped in the routine FBC.”
He huffed. I sighed.
“Okay, I’ll tell the team,” He said and hung up. I put the sample back in the rack and the phone in its holder.
“What was that about?” Asked the senior in the lab. I explained the situation to her and also told her that the haematology registrar would be calling back later to confirm the new and hopefully accurate results.
“Well they shouldn’t be sending citrated samples anyway. This is their fault,” she said.
I raised my eyebrows and puckered my lips. “That’s fair enough, but if we’ve received a sample we should at least deal with it appropriately. Processing an underfilled citrate sample is a failure on the lab.” I retorted.
“But..” she began.
“It’s well after the end of my shift time, I’ve given you a heads up that they’ll be sending another sample and now I am going home.” I had no time for the blame game. As a strong believer in people taking accountability for their actions, this conversation was going down a path I really could not be bothered with.
Whenever such scenarios occur and the finger pointing begins, there are always winners and losers. Who’s in the right? Who’s in the wrong? Who cares? We should focus on our own processes and not palm off our own mistakes to others. Because ultimately the only one who really loses in such scenarios is the patient.
Privacy Policy | Refund & Return Policy | Only Cells LTD © 2025
One Comment
This post offers a thought-provoking exploration of the ‘winners and losers’ in the context of healthcare where you’d only assume there to be winners. It is interesting how easily and quickly people are quick to find solutions by blaming others, as that senior in the story did rather than also take responsibility from the lab perspective. I really liked the final line about in the end, it is the patient who loses.